The latest technique that coats anticancer drugs in membranes made from a patient’s own platelets has been discovered. It allows the drugs to last longer in the body and attack both primary cancer tumors and the circulating tumor cells that can cause a cancer to metastasize .The work was tested successfully in an animal model. “There are two key advantages to using platelet membranes to coat anticancer drugs,” says Zhen Gu, corresponding author of a paper on the work and an assistant professor in the joint biomedical engineering program at North Carolina State University and the University of North Carolina at Chapel Hill.
“First, the surface of cancer cells has an affinity for platelets, they stick to each other. Second, because the platelets come from the patient’s own body, the drug carriers aren’t identified as foreign objects, so last longer in the bloodstream. This combination of features means that the drugs can not only attack the main tumor site, but are more likely to find and attach themselves to tumor cells circulating in the bloodstream and essentially attacking new tumors before they start,” says Quanyin Hu, lead author of the paper and a Ph.D. student in the joint biomedical engineering program.
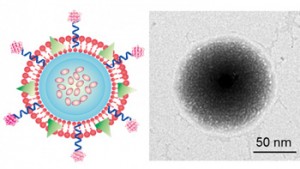
Researchers started by taking blood from the mice and isolating platelets in order to separate their membranes. The membranes are then placed in a solution with nanoscale gel that includes the cancer drug doxorubicin. The solution is compressed, which forces the gel and drug through the membrane, creating nanospheres that are finally treated with another cancer drug, TRAIL. The two drugs work in tandem, as TRAIL attacks the membranes of cancer cells and doxorubicin attacks the nucleus of cancer cells. When the platelets come into contact with a tumor, the platelets bind to the surface of cancer cells. TRAIL on the outside of the platelets attacks the cancer cell’s membrane, causing the nanosphere pseudo-platelet to be swallowed by the cancer cell. Once inside, the nanosphere is broken apart and the hidden doxorubicin attacks the cancer cell’s nucleus, killing it.
In the research in mice, not only did the platelet-containing nanospheres remain in their bodies for 30 hours, as compared to 6 for the gel alone, but were far more effective against large tumors, the researchers reported. When one of the pseudo-platelets comes into contact with a tumor, three things happen more or less at the same time. First, the P-Selectin proteins on the platelet membrane bind to the CD44 proteins on the surface of the cancer cell, locking it into place. Second, the TRAIL on the pseudo-platelet’s surface attacks the cancer cell membrane. Third, the nanoscale pseudo-platelet is effectively swallowed by the larger cancer cell. The acidic environment inside the cancer cell then begins to break apart the pseudo-platelet, freeing the Dox to attack the cancer cell’s nucleus.
“We’d like to do additional pre-clinical testing on this technique,” Gu says. “And we think it could be used to deliver other drugs, such as those targeting cardiovascular disease, in which the platelet membrane could help us target relevant sites in the body.”
For more information please visit: www.ncsu.edu