Since their discovery in the 1920s, antibiotics have transformed our ability to treat infections. As antibiotic resistance increases, these lifesaving drugs do not work as well as they once did, and successfully treating common infections becomes more difficult.
Antibiotic resistance is a growing problem, both in the United States and across the world. The main driving factors behind antibiotic resistance are the overuse and misuse of antibiotics. Learn more below about when antibiotics are and are not needed for common infections, and the potential harms of using antibiotics.
If You Have a Cold or Flu, Antibiotics Won’t Work for You
Are you aware that colds, flu, most sore throats, bronchitis, and many sinus and ear infections are caused by viruses? Did you know that antibiotics do not help fight viruses? It’s true. For the overwhelming majority of common respiratory infections, antibiotics are not helpful.
Antibiotics cure bacterial infections, not viral infections such as:
Colds or flu
Most coughs and bronchitis
Most sore throats
Runny noses
Taking antibiotics for viral infections will not:
Cure the infection
Keep other individuals from catching the illness
Help you feel better
Antibiotics Can Cause More Harm than Good
Taking antibiotics when you have a virus may do more harm than good:
Antibiotics are responsible for 1 out of 5 emergency department visits for adverse drug events. Antibiotics are the most common cause of emergency department visits for adverse drug events in children under 18 years of age.Offer a click to view larger image option
Taking antibiotics increases your risk of getting an antibiotic-resistant infection later.
Antibiotics kill the healthy bacteria in the gut, allowing more harmful bacteria, such as C. difficile, to grow in its place.
Although this infection is more commonly found in hospitals, it also occurs in clinics outside of the hospital

Underlying the phenotypic mechanisms of antibiotic resistance are the genetics of antibiotic resistance. Bacteria, like other living organisms, possess DNA that codes for the proteins and enzymes it requires for survival. Changes to the DNA can result in alterations in the final proteins or enzymes, which in turn can lead to antibiotic resistance. A common genetic mechanism for the development of antibiotic resistance is the acquisition of tiny fragments of DNA known as plasmids or transposons. Transposons may code for a specific antibiotic-inactivating enzyme, which, when produced by the bacteria, destroys an incoming antibiotic before it has an opportunity to work. These tiny fragments may be passed directly from one bacterium to another by a process known as conjugation. Alternatively, small viruses may attack certain bacteria and inject DNA fragments by a process known as transduction.
Another genetic mechanism of antibiotic resistance is the acquisition and accumulation of resistance genes from neighboring bacteria through a process known as transformation. A good example of this is the pneumococcus bacterium, which is a common cause of pneumonia, bacterial sinusitis, middle ear infections and even meningitis. When penicillin first became available for clinical use in the 1940s, the pneumococcus bacterium was 100 percent susceptible to penicillin. After decades of use, a portion of pneumococcal bacteria have accumulated small pieces of genetic material that they have scavenged from other bacteria, rendering them resistant to the effects of penicillin. Finally, a fourth genetic mechanism by which bacteria can develop antibiotic resistance is through mutations in their DNA. Every time a bacterium multiplies and grows, it may develop a mutation in its DNA. If the mutation occurs in a part of the DNA that codes for a protein or substance that is the target of an antibiotic, the bacteria may become resistant to that drug.
There is nothing stopping a bacterium from becoming resistant to more than one antibiotic. In fact, for some bacteria and antibiotics, cross resistance is common, which creates a new problem. The more drugs a bacterium is resistant to, the more difficult it becomes to treat an infection. Although many alternative antibiotics are currently available for use and new ones continue to be developed, there is a concern that doctors may run out of options for treating some highly resistant bacterial infections. Newer antibiotics may also be more costly than older ones and could come with side effects that make them more difficult to take. Ultimately the biggest concern with antibiotic resistance is that a patient will be treated for a potentially life threatening infection such as meningitis with an antibiotic to which the underlying bacteria is resistant. By the time the resistance is recognized through laboratory testing the patient may have suffered severe consequences.
The hope is that with more appropriate use of antibiotics and thus a reduction in antibiotic selection pressure, we can stem the tide of resistance and maintain a useful armamentarium of antibiotics for treating all types of bacterial infections. Patients should thus avoid taking antibiotics for things such as the common cold (which is caused by viruses and not bacteria), complete their courses of antibiotics as prescribed and not share their antibiotics with others.
Never take an antibiotic for a viral infection like a cold or the flu. Antibiotics do NOT cure viral infections such as:
Colds
Flu
Most sore throats
Most coughs and bronchitis (“chest colds”)
Many sinus infections
Many ear infections
Never pressure your healthcare professional to prescribe an antibiotic.
Never skip doses or stop taking an antibiotic early, even if you no longer feel sick, unless your healthcare professional tells you to do so.
Never save antibiotics for the next time you become sick and do not take antibiotics prescribed for someone else.
Taking the wrong medicine may delay correct treatment, allow bacteria to multiply, and cause unwanted or severe side effects. Discard any leftover medication.
- Antibiotic resistance has been called one of the world’s most pressing public health problems.
- Every time a person takes antibiotics, sensitive bacteria are killed, but resistant ones may be left to grow and multiply.
- Repeated and improper uses of antibiotics are the primary causes of the increase in drug-resistant bacteria.
- Overuse and misuse of antibiotics threatens the usefulness of these important drugs. Decreasing inappropriate antibiotic use is a key strategy to control antibiotic resistance.
- Antibiotic resistance in children is of particular concern because they have the highest rates of antibiotic use and often have fewer antibiotic choices since some antibiotics cannot be safely given to children.
- Antibiotic resistance can cause significant suffering for people who have common infections that once were easily treatable with antibiotics.
- When antibiotics do not work, infections often last longer, cause more severe illness, require more doctor visits or extended hospital stays, and involve more expensive and toxic medications. Some resistant infections can even cause death.
Newly identified gene that renders bacteria resistant to polymyxin antibiotics—drugs often used as the last line of defense against infections—has the potential to be shared between different types of bacteria. The finding raises concern that the transferable gene could make its way into infectious bacteria that are already highly resistant to drugs, thereby creating strains of bacteria immune to every drug in doctors’ arsenal.
The gene, dubbed mcr-1, exists on a tiny, circular piece of DNA called a plasmid. These genetic elements, common among bacteria, are mobile; bacteria can make copies of them and share them with whatever bacteria happens to be nearby. Though scientists have previously discovered genes for polymyxin resistance, those genes were embedded in bacterial genomes, thus were not likely to easily spread.
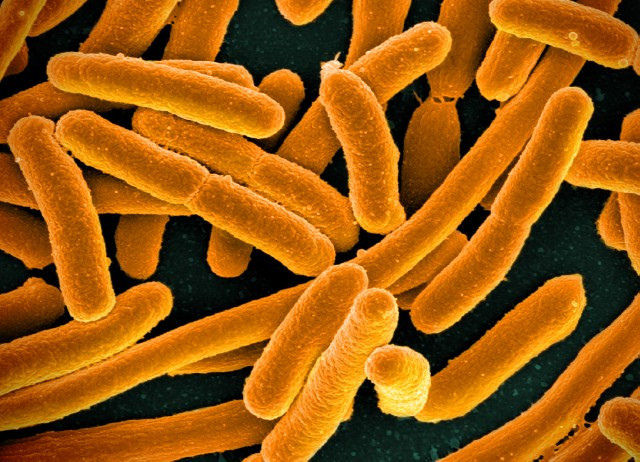
In a study, published Wednesday in the Lancet Infectious Diseases, researchers in China report first finding the mcr-1-containing plasmid in Escherichia coli bacteria isolated from a pig. The plasmid was solely responsible for the bacteria being resistant to colistin, a type of polymyxin commonly used in animals in China, but less so in the US and Europe. On further examination, the researchers also found mcr-1-containing plasmids in E. coli and Klebsiella pneumoniae isolated from a small number of patients in hospitals in Guangdong and Zhejiang provinces.
Lab tests showed that the plasmid could easily move between E. coli strains, transforming polymyxin-sensitive strains into polymyxin-resistant ones. But, the plasmid had a harder time moving between different bacterial species. The researchers had to coax the plasmid into other species by zapping bacterial cells with an electrical pulse to make their membranes more permeable—a technique called electroporation. The finding suggests that the plasmid may not easily move between species naturally.
Still, the authors cautioned that if mcr-1 containing plasmids spread to multi-drug resistant bacterial strains, it could make them “truly pan-drug resistant,” and resulting infections would be untreatable.
