A tiny wireless subretinal implant called PRIMA—a photovoltaic microchip placed beneath the retina and used with a camera-equipped pair of glasses and a pocket processor—has been shown in a multicenter clinical trial to partially restore functional central vision in patients with geographic atrophy (advanced “dry” AMD). At 12 months many trial participants could read letters, numbers and words using the system; mean gains on a standard ETDRS chart were large and clinically meaningful.
A retinal implant developed by Science Corp. has for the first time restored some functional vision to patients with a severe form of age-related macular degeneration (AMD), a common eye disease and the leading cause of blindness in older adults, according to a new study.
Geographic atrophy (GA) from age-related macular degeneration progressively destroys the light-sensing photoreceptors in the macula, the retinal region responsible for high-acuity central vision (reading, face recognition, fine detail). Patients with advanced GA retain peripheral vision but lose central vision; until now there has been no therapy that reliably restores meaningful central vision once the macula is extensively atrophic. The PRIMA approach aims to replace the lost function of photoreceptors by electrically stimulating the remaining inner retinal neurons to evoke patterned visual percepts.
What PRIMA is — hardware and system architecture
The PRIMA system is a three-part prosthetic-vision platform that replaces the function of lost photoreceptors:
Subretinal photovoltaic implant (the chip)
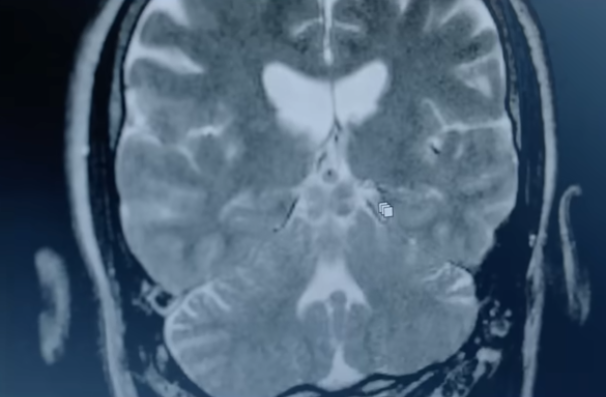
A tiny wireless microchip implanted beneath the retina (reported device size ≈ 2 mm × 2 mm, extremely thin). The chip contains an array of photovoltaic pixels (published sources cite ~378 photovoltaic pixels/cells for the version used in clinical studies). Each pixel converts pulsed near-infrared light projected onto the retina into a local electric current. These microcurrents stimulate the secondary retinal neurons (bipolar cells), thereby producing patterned activation that can be perceived as points/lines by the visual system.
Glasses with a scene camera and projector
A head-mounted camera captures the scene. The video feed is processed (image enhancement / encoding) and then projected as patterned near-infrared illumination onto the eye containing the implant. Because the implant is photovoltaic and wireless, it does not need an implanted power lead—the projected light both encodes the image and powers the pixels.
Processes the camera frames, transforms them into stimulation patterns adjusted for the implant geometry and the patient’s mapping, and controls timing/intensity sent to the projector. Rehab sessions calibrate the mapping between projected patterns and the patient’s percepts.
Photovoltaic pixels are arranged in a high-density array; each pixel behaves like a tiny light-to-current converter. The system uses pulsed near-infrared to avoid stimulating the remaining natural photoreceptors and to maximize implant coupling.
The implant stimulates inner retinal neurons (bipolar cells) directly, bypassing lost photoreceptors but utilizing downstream retinal circuitry and the optic nerve to send patterned signals to the brain. This is a subretinal approach (implant sits between the retinal pigment epithelium and the neural retina).
Surgical procedure and immediate postoperative course
- Implantation is a vitreoretinal surgical procedure performed by experienced retinal surgeons. The chip is inserted under the retina into the macular area through a small retinotomy and positioned at the foveal region. Reported implantations were typically under two hours in experienced hands. After a short recovery period (weeks), the patient begins prosthetic training with the glasses.
Rehabilitation & how patients learn to use it
- Restored vision is prosthetic and requires training: the brain must learn to interpret the patterned stimulation; early gains are often modest and improve over weeks-to-months of training. Trial participants used the system at home for tasks such as reading large letters, numbers and—after training—even words. Intensive, guided visual rehabilitation is therefore an integral part of successful outcomes.
Safety and adverse events
- The NEJM paper reports safety data at 12 months: no systemic safety signals and no large declines in the remaining peripheral (natural) vision on average. Surgical complications are possible (as with any retinal surgery) and the system requires monitoring, but reported safety in the trial was acceptable for this stage. Detailed device-specific adverse events and rates are provided in the NEJM manuscript.
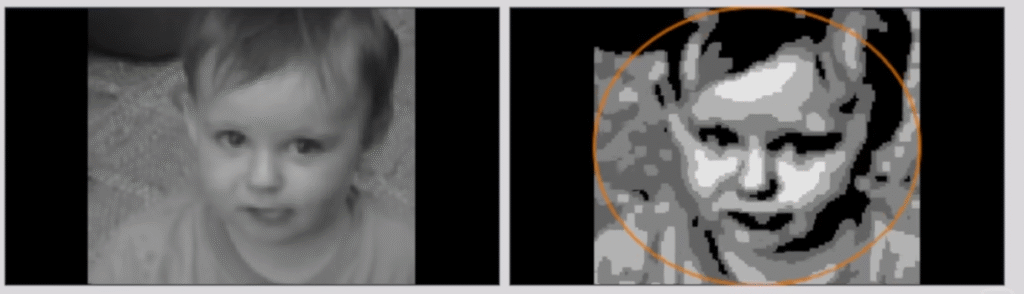
First demonstration of “functional central vision” restoration for advanced GA: unlike prior retinal prostheses aimed at retinitis pigmentosa or wide-field low-resolution perception, PRIMA has shown the ability to restore useful central visual functions (reading letters/words) in patients whose macula was destroyed by GA. This addresses a major unmet need because GA is common and disabling among older adults.
Wireless photovoltaic approach avoids implanted power leads—simplifying surgical design and reducing hardware footprint. The subretinal photovoltaic concept is an elegant engineering solution: collocate energy capture and stimulation at the site of action (photovoltaic pixels under the retina).
The PRIMA subretinal photovoltaic BCI system marks a major technical and clinical milestone: for the first time, a small wireless implanted microchip plus external camera/processor delivered clinically meaningful central vision—enough for many trial participants to read letters and numbers—after years of incurable central vision loss from geographic atrophy. While challenges remain (resolution limits, training needs, long-term data, and broad access), the NEJM-reported results represent a real step change in what’s achievable with retinal prostheses and neural engineering.
The multi-center clinical trial evaluated the PRIMA implant system in 38 patients across 17 clinical sites in five countries. The key findings include:
Mean improvement of 25.5 letters (more than 5 lines) on ETDRS letter chart.
84% of patients reported the ability to read letters, numbers, and words, restoring functional central vision.
80% of patients achieved significant prosthetic visual acuity improvements of at least logMAR 0.2 (equivalent to 10 letters on ETDRS chart) at 12 months (p<0.001).
No significant decline in mean existing peripheral natural vision was observed.
The implant can be safely implanted under the atrophic macula. “Serious adverse events” occ
Macular degeneration steals sight. A chip implant may get it back.
Eye prosthesis is the first to restore sight lost to macular degeneration
