Handheld, miniature microscope being developed by University of Washington mechanical engineers could allow surgeons to “see” at a cellular level in the operating room and determine where to stop cutting.
The new technology, developed in collaboration with Memorial Sloan Kettering Cancer Center, Stanford University and the Barrow Neurological Institute, is outlined in a paper published in January in the journal Biomedical Optics Express.
The handheld microscope, roughly the size of a pen, combines technologies in a novel way to deliver high-quality images at faster speeds than existing devices. Researchers expect to begin testing it as a cancer-screening tool in clinical settings next year.

UW mechanical engineering doctoral students and assistant professor Jonathan T.C. Liu work to align a handheld microscope for cancer detection in patients. From left to right: Ye Chen, Linpeng “Peter” Wei, Liu and Chengbo Yin.Dennis Wise, University of Washington
That process subjects patients to an invasive procedure and overburdens pathology labs. A miniature microscope with high enough resolution to detect changes at a cellular level could be used in dental or dermatological clinics to better assess which lesions or moles are normal and which ones need to be biopsied.
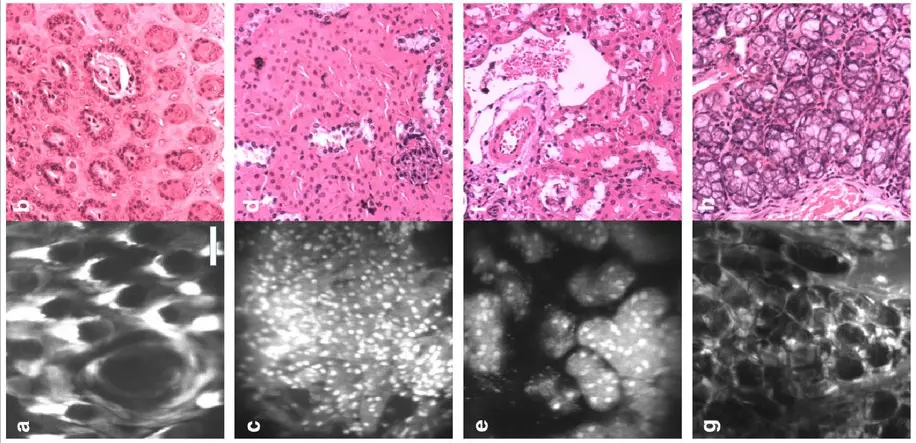
The new microscope revealed by UW is able to combine technologies in a compact and novel way, generating high-quality images at faster speeds than existing bulkier devices. It uses “dual-axis confocal microscopy” to illuminate and more clearly see through opaque tissue, capturing details up to half a millimetre beneath the tissue surface, where some types of cancerous cells originate. In the video below, for example, the team produced images of fluorescent blood vessels in a mouse ear. In their paper, they demonstrate how their invention has sufficient resolution to see subcellular details.
“For brain tumour surgery, there are often cells left behind that are invisible to the neurosurgeon. This device will really be the first to let you identify these cells during the operation and determine exactly how much further you can reduce this residual,” said project collaborator Nader Sanai, a professor of neurosurgery at the Barrow Neurological Institute in Phoenix. “That’s not possible to do today.”
