A new system can convert MRI scans into 3D-printed, physical models in a few hours.
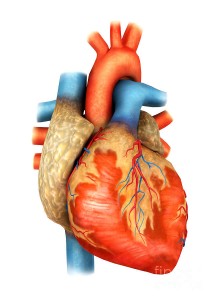
Researchers at MIT and Boston Children’s Hospital have developed a system that can take MRI scans of a patient’s heart and, in a matter of hours, convert them into a tangible, physical model that surgeons can use to plan surgery.
The models could provide a more intuitive way for surgeons to assess and prepare for the anatomical idiosyncrasies of individual patients.
MRI data consist of a series of cross sections of a three-dimensional object. Like a black-and-white photograph, each cross section has regions of dark and light, and the boundaries between those regions may indicate the edges of anatomical structures. Determining the boundaries between distinct objects in an image is one of the central problems in computer vision, known as “image segmentation.” However, general-purpose image-segmentation algorithms aren’t reliable enough to produce the very precise models that surgical planning requires.
Typically, the way to make an image-segmentation algorithm more precise is to augment it with a generic model of the object to be segmented. Human hearts, for instance, have chambers and blood vessels that are usually in roughly the same places relative to each other. That anatomical consistency could give a segmentation algorithm a way to weed out improbable conclusions about object boundaries. The problem with that approach is that many of the cardiac patients at Boston Children’s Hospital require surgery precisely because the anatomy of their hearts is irregular. Inferences from a generic model could obscure the very features that matter most to the surgeon.
In the past, researchers have produced printable models of the heart by manually indicating boundaries in MRI scans but with the 200 or so cross sections in high-precision scans, that process can take eight to 10 hours. Researchers asked a human expert to identify boundaries in a few of the cross sections and allow algorithms to take over from there. Their strongest results came when they asked the expert to segment only a small patch, one-ninth of the total area of each cross section. In that case, segmenting just 14 patches and letting the algorithm infer the rest yielded 90 percent agreement with expert segmentation of the entire collection of 200 cross sections. Human segmentation of just three patches yielded 80 percent agreement.
The human segmentation of sample patches and the algorithmic generation of a digital, 3-D heart model takes about an hour. The 3-D-printing process takes a couple of hours more. Currently, the algorithm examines patches of unsegmented cross sections and looks for similar features in the nearest segmented cross sections. Researchers believe that its performance might be improved if it also examined patches that ran obliquely across several cross sections. This and other variations on the algorithm are the subject of ongoing research.
The clinical study in the fall will involve MRIs from 10 patients who have already received treatment at Boston Children’s Hospital. Each of seven surgeons will be given data on all 10 patients, some probably, more than once. That data will include the raw MRI scans and, on a randomized basis, either a physical model or a computerized 3-D model, based, again at random, on either human segmentations or algorithmic segmentations
Using that data, the surgeons will draw up surgical plans, which will be compared with documentation of the interventions that were performed on each of the patients. The hope is that the study will shed light on whether 3-D-printed physical models can actually improve surgical outcomes.
Surgeons definitely believe that a 3-D model would indeed help as they have used this type of model in a few patients, and in fact performed ‘virtual surgery’ on the heart to simulate real conditions.
Doing this really helped with the real surgery in terms of reducing the amount of time spent examining the heart and performing the repair. Having this will also reduce the incidence of residual lesions and imperfections in repair by allowing to simulate and plan the size and shape of patches to be used Ultimately, 3D-printed patches based upon the model will allow doctors to tailor prosthesis to individual patients and also get a better visual.
Many patients and families have commented that this empowers them to understand their condition better.
For more information please visit: www.news.mit.edu