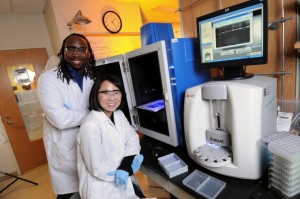
Researchers at the Georgia Institute of Technology have developed a predictive model that can provide doctors with an “invasiveness index” for cancer based on blood samples from individual patients, according to a new study. The test is based on chemical expression by specific cells in the body that help cancer move from the breast to other parts of the body.
We want women to have more information to make a personal decision beyond the averages calculated for an entire population,” said Manu Platt, an associate professor at Georgia Tech University, in a press release. “We are using our systems biology tools and predictive medicine approaches to look at potential markers we could use to help us understand the risk each woman has. This would provide information for a more educated discussion of treatment options.”
The researchers have been developing a method of measuring the variability in macrophage expression of four types of cathepsin, the cathepsin inhibitor cystatin C, and kinase activation levels, which are significant to the assistance of tumors to spread beyond the breast. Using macrophages from monocytes donated by healthy women, the researchers tested the technique using a standard breast cancer cell line. Using a gel to simulate breast tissue, they measured the levels of protein expression by the macrophages against the number of cancer cells which invaded it.
To test it with real patients, the researchers obtained blood tests from 9 women being treated for breast cancer at DeKalb Medical Center in Atlanta, finding that their method correlated with the diagnoses their doctor had made. In addition to testing the method further, Platt said the researchers will follow the 9 women for 5 years to determine if the test also was relevant to the potential for cancer recurrence. “We are measuring at the level of activity of these intracellular enzymes and the ultimate activity of the proteases they produce that are not only the biomarkers of the tumor, but also help the tumor grow,” Platt said. “Everything about us is different. Our genetics are different and our lifestyles are different, so clinicians have to make decisions in all that variability. All of those differences can be measured and captured in this output.”
Being obese or overweight is the second leading of cancer incidence in country, right behind tobacco use, according to the American Association of Cancer Research. Smoking accounts for about 33 percent of cancer cases in country, while being overweight results in about 20 percent. This is particularly troubling for women at risk of breast cancer, Dr. Kristen Fernandez, director of the breast center at MedStar Franklin Square Medical Center. “The two biggest risk factors for getting breast cancer are being a woman and getting older,” Fernandez began, sitting in a tranquil waiting area outside of the breast center at Franklin Square. “There’s absolutely nothing you can do about those two. We hope that you continue to get older. We want you to live into old age but she said essential steps for women to lessen the possibility of contracting cancer is to maintain a healthy body weight and exercise.”
“Obesity has been directly linked to an increase risk of breast cancer,” Fernandez said.” Even women who aren’t at their ideal body weight, if they exercise, it lowers their risk of breast cancer. “She recommended women work out for about 30 to 40 minutes a day, five to six days a week. “Not only does it help you drop weight but it changes the hormonal milieu in your body,” Fernandez said. “Obesity is linked to breast cancer because the peripheral fat cells in your body actually make a precursor to estrogen. It’s converted to estrogen by your adrenal glands, which sit on your kidneys. By decreasing the fat cells, you’re decreasing the estrogen production and in a sense lowering the breast cancer risk.”
The American Association of Cancer Research in its annual Cancer Progress Report ranked the top six preventable causes of cancer, Smoking (Tobacco use), accounts for 33 percent, Obesity, accounts for 20 percent, Cancer-causing pathogens, accounts for 16 percent, Insufficient physical activity, accounts for 5 percent, Poor dietary habits, account for 5 percent and Tanning (Exposure to UV light from the sun), accounts for 2 percent
The American Association of Cancer Research this year painted a clearer picture of breast cancer detection. “In June 2014, the FDA approved a new contrast agent to use with MRI to assess to presence and extent of cancer within the breasts. This decision was made after results of two larger clinical trials showed that the new contrast age, gabobutrol, significantly improved The ability of MRI to clearly visualize cancer in the breast,” according to the association’s annual progress report. Fernandez said getting a yearly mammogram is the most important thing women can do to catch cancer as early as possible. Women should start getting breast screenings when they turn 40, a fact Fernandez said is overlooked by some women. “Everyone has excuses. ’Oh, I heard mammograms don’t find all cancers.’ Well they don’t. But they still find 80 to 90 percent of cancers depending on your age group. To not get one at all, you’re going to be missing 100 percent,” she said offering a nudge toward one more avenue to prevent perhaps a more serious case of breast cancer.
For more information please visit: www.rh.gatech.edu